Key features
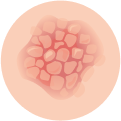
Plaques
The most common sign of psoriasis is the formation of thick, raised, and inflamed skin patches. Additionally, these plaques often appear red or pink and are covered with silver or white scales. Furthermore, they can be itchy, painful, and, in severe cases, may crack or bleed.
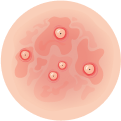
Nail changes
Psoriasis can affect the nails, causing pitting (small dents), discoloration, thickening, and separation of the nail from the nail bed. In some cases, nails may become crumbly or develop ridges.
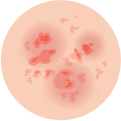
Scalp involvement
Psoriasis frequently affects the scalp, leading to the formation of scaly patches or dandruff-like flakes. It can cause itching and discomfort and may extend to the forehead, neck, or behind the ears.
Joint inflammation
Some individuals with psoriasis may develop a related condition called psoriatic arthritis, which causes joint pain, stiffness, and swelling. Psoriatic arthritis can affect any joint in the body and may lead to significant joint damage if left untreated.
Triggers
Certain factors can trigger or worsen psoriasis flare-ups. These triggers can vary among individuals and may include stress, infections, injury to the skin, certain medications (such as beta-blockers or lithium), cold and dry weather, smoking, and alcohol consumption.
Emotional impact
Psoriasis can have a significant impact on an individual’s emotional well-being. It may cause feelings of self-consciousness, embarrassment, frustration, or low self-esteem. Psychological support and counseling can be helpful in managing the emotional aspects of living with psoriasis.